IV Therapy Compliance: Who Can Legally Administer IV Drips in Your Clinic
The booming popularity of IV therapy has transformed wellness and aesthetic clinics nationwide. From vitamin drips to NAD+ infusions, patients now view IV therapy as a routine part of self-care. But as the market grows, so does scrutiny from regulators. IV therapy compliance is no longer optional, it is the legal foundation of whether your clinic can safely and lawfully offer these treatments.
Why IV Therapy Compliance Matters
IV drips involve directly infusing substances into the bloodstream. This is not a spa service, it is a medical procedure with risks such as infection, electrolyte imbalance, or fluid overload. Without proper oversight, the consequences can be severe, even fatal.
IV therapy compliance ensures:
- Patient safety through legitimate medical orders and qualified staff.
- Clinic protection from liability, insurance denials, and malpractice claims.
- Regulatory alignment with state medical boards and federal standards.
- Professional credibility in a competitive wellness market.
In 2025, IV therapy compliance is under the microscope more than ever. States are updating laws, insurance carriers are tightening requirements, and patients are becoming more aware of the need for medically supervised care.
The Legal Foundation of IV Therapy Compliance
At the heart of IV therapy compliance are three questions every clinic must answer:
- Who can issue the order for IV therapy?
- Who can legally administer the IV drip?
- What documentation and agreements are required?
1. Orders Must Come From Licensed Providers
Across the U.S., IV therapy must be ordered by a licensed physician (MD or DO), nurse practitioner (NP), or physician assistant (PA). Standing orders (“all patients get XYZ drip”) are explicitly prohibited in many states. Instead, each IV therapy session must be tied to a patient-specific order, documented after a legitimate provider–patient interaction.
2. Only Qualified Staff Can Administer IV Therapy
Administration of IV drips is not a task for medical assistants or unlicensed staff. Laws like Jenifer’s Law in Texas make it clear: only RNs, NPs, or PAs may start and monitor IV infusions.
This standard protects patients and shields clinics from serious penalties. Allowing unqualified staff to perform IV therapy is considered practicing medicine without a license, and it exposes both the supervising physician and the clinic to liability.
3. Written Delegation and Supervision Agreements
In most states, physicians who delegate IV therapy to RNs, NPs, or PAs must create formal supervision agreements and administration protocols. These documents define:
- Which practice locations are covered
- Which medications and infusions are authorized
- What emergency protocols are in place
- How often reviews and updates occur
Many states also require these agreements to be filed with the medical board as part of transparent compliance oversight.
The Role of Telehealth in IV Therapy Compliance
Modern clinics are increasingly leveraging telehealth to streamline compliance while scaling services. Platforms like Qualiphy allow clinics to:
- Conduct Good Faith Exams (GFEs) or Patient Specific Orders (PSOs) through live video or secure asynchronous platforms.
- Connect patients instantly with licensed providers in their state.
- Generate compliant documentation stored securely in EMRs.
- Route prescriptions and IV therapy orders to partner pharmacies for safe fulfillment.
This digital infrastructure eliminates guesswork. Instead of relying on outdated standing orders, clinics can integrate IV therapy compliance directly into workflows, ensuring every drip is supported by a provider-signed medical order.
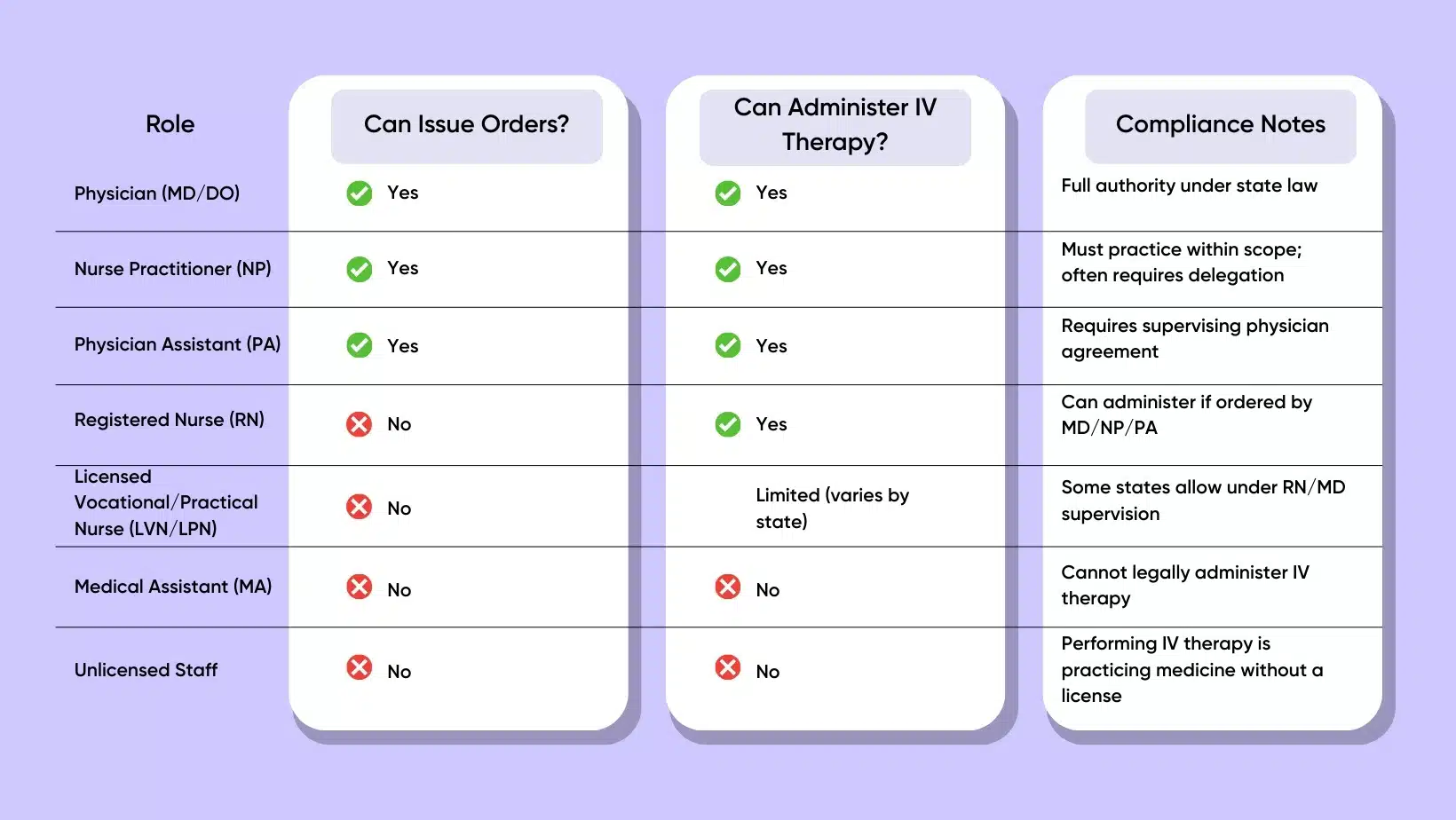
Who Can Legally Administer IV Therapy: A Role-by-Role Breakdown
Here’s a clear look at who is legally allowed to participate in the IV therapy process
Documentation: The Backbone of IV Therapy Compliance
Strong documentation is what separates compliant clinics from risky operators. Key documents include:
- Good Faith Exams (GFEs): Initial provider–patient consultations, often required before ordering therapy.
- Patient Specific Orders (PSOs): Individualized orders tied to a specific patient and treatment.
- Delegation Agreements: Physician-signed documents outlining scope of care, supervision, and emergency protocols.
- Telehealth Records: Secure notes of live or form-based encounters, stored for audits and insurance verification.
Without these, a clinic is exposed to malpractice claims, audits, or board actions.
Penalties for Ignoring IV Therapy Compliance
Non-compliance is costly. Consequences include:
- Regulatory penalties: State boards can suspend licenses or impose fines.
- Insurance denials: Carriers may refuse claims if compliance protocols aren’t followed.
- Civil liability: Patients harmed by non-compliant IV therapy can sue for damages.
- Criminal charges: In extreme cases, clinics may face charges for practicing medicine without a license.
The takeaway: the cost of non-compliance far exceeds the effort of building compliant systems.
Building a Culture of Compliance in Your Clinic
Compliance is not just a checklist, it’s a culture. Clinics that thrive in the long term view IV therapy compliance as integral to growth. Here’s how to build it:
- Audit your current protocols. Identify if standing orders, unqualified staff, or missing documentation are creating risks.
- Train your team. Ensure every staff member knows who can and cannot administer IV therapy.
- Adopt compliant telehealth tools. Platforms designed for aesthetics and wellness can streamline provider access and documentation.
- Update delegation agreements annually. Laws and protocols change, make sure your paperwork does too.
Market compliance as a strength. Patients are more likely to choose clinics that highlight safety and regulatory alignment.
The Future of IV Therapy Compliance
The regulatory environment is tightening. Just as telehealth moved from optional to essential for Good Faith Exams, IV therapy compliance is evolving from a “best practice” to a legal necessity.
Future trends include:
- Nationwide adoption of PSOs as the baseline for IV therapy orders.
- Stricter oversight of med spas offering elective IV therapy.
- Integration of compliance automation through AI-driven telehealth platforms.
- Greater accountability for supervising physicians in multi-state operations.
Clinics that invest in compliance today will be positioned as leaders tomorrow, trusted by patients, insurers, and regulators alike.
Conclusion
IV therapy has become a cornerstone of modern wellness and aesthetics, but it is not without risk. Ensuring IV therapy compliance protects patients, shields clinics from liability, and positions practices for sustainable growth.
The rules are clear: only licensed providers can order IV therapy, and only qualified clinicians (RNs, NPs, PAs) can administer it. Written agreements, telehealth consultations, and patient-specific orders are no longer optional; they are the legal foundation of safe practice.
By embracing a compliance-first approach, your clinic doesn’t just avoid penalties; it builds patient trust, scales services with confidence, and secures its place in the future of aesthetic medicine.
FAQs About IV Therapy Compliance